
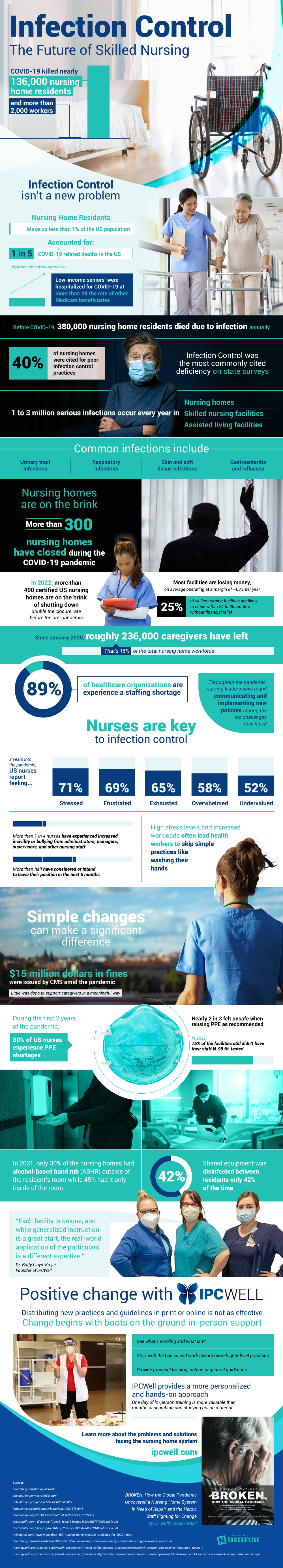
The COVID-19 pandemic is notorious for the damage it caused across the healthcare industry at large. Disproportionately still, nursing homes were affected. Representing only 1% of the population nursing home residents managed to make up a fifth of all COVID deaths.
This is due, in large part, to the struggle in infection control policies. While other compounding factors like closing homes and a lack of profitability are certainly influential, the nurses of these homes are the single largest influencing factor.
Since 2020, 15% of the nursing home workforce has quit. This has created massive shortages, only increasing the stress put on the remaining workforce. This then works to reduce the quality of care the remaining workforce is giving, an unfortunately vicious cycle.
Still, this is not an issue without hope. While certainly working to provide more resources to existing nursing homes is essential, there are smaller steps that can be made in conjunction as well. Specifically on the ground training and reevaluation with these nurses is essential.
There are countless online materials to help nurses, but actually getting someone there to look at what’s working and what’s not is invaluable. Overworked nurses aren’t going to have the time or energy to revamp systems, but that’s where others can come in to help. Organizations like IPCWell work with this explicit purpose, for example.
It’s certainly no universal fix to the issue, but healthcare workers can use all the help they can get. The effects of COVID weren’t too dramatic for many, but for those inside nursing homes, residents and workers alike, it has been one of the most important forces in their lives. Learn more about the way forward through proper infection control protocol in the visual deep dive below:
Source: IPCWell.com




